Medical Sciences 6: 66 [with Mette Kjer Kaltoft] PMID: 30135365 DOI: 10.3390/medsci6030066
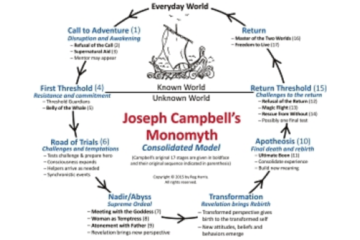
Cultural changes are needed in medicine if the benefits of technological advances are to
benefit healthcare users. The Digital Health Manifesto of ‘medical futurist’ doctor Bertalan Meskó and
‘e-patient’ Dave deBronkart, The Patient Will See You Now by Eric Topol and The Patient as CEO by
Robin Farmanfarmaian, are among the proliferating warnings of the approaching paradigm shift
in medicine, resulting, above all, from technological advances that gives users independent access
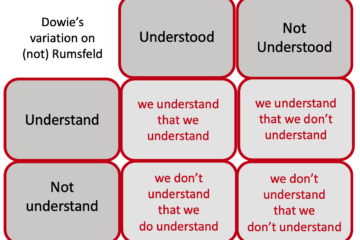
to exponentially increasing amounts of information about themselves. We question their messages
only in suggesting they do not sufficiently shift the focus from ‘patient’ to ‘person’ and consequently
fail to recognise the need for the credible, efficient, ethical and independent decision support that
can ensure the ‘democratisation of knowledge’ is person empowering, not overpowering. Such
decision support can ensure the ‘democratisation of decision,’ leading to higher quality decisions
and fully-informed and preference-based consent to health provider actions. The coming paradigm
will therefore be characterised by apomediative (‘direct-to-consumer’) decision support tools, engaged
with by the person in the community to help them make health production decisions for themselves
(including whether to consult a healthcare professional or provider), as well as intermediative
(‘direct-from-clinician’) tools, delivered by a health professional in a ‘shared decision making’
or ‘co-creation of health’ process. This vision paper elaborates on the implementation of these
preference-sensitive decision support tools through the technique of Multi-Criteria Decision Analysis.
Current training curricula and practice arrangements, as well as attitudes, reflect a culture that has not yet acknowledged the inevitably disruptive effects of citizen-empowering technological change. That technological changes mandate cultural changes is accordingly the central message of the Manifesto. Attempts to absorb these innovative technologies into the current culture—as just new ways to do old things—are doomed to fail and the
blame will be improperly placed on the technology not fitting into the status quo culture, rather than
the culture not changing to enable the benefits of the technology to be realised.
…in calling for cultural change, the Manifesto authors underestimate the massive material
interests embedded in the present paradigm, in the form of personal and collective capital, both
financial and professional. These material interests underpin the resistance to change which most often
manifests itself in the broad claim that the suggested changes, while appealing in principle, will not be
in the true interests of ‘our patients’ in practice.
The new paradigm must therefore involve the creation of genuinely independent resource bases for person-driven health production and co-creation, accessible and delivered ‘direct-to-consumer/user/person/citizen.’
Following Eysenbach, we refer to these resources as ‘apomediative,’ because they ‘stand by’
the person but ‘away from’ (apo-) and independent of the provider of the good or service in question.
Familiar examples of apomediative services are the multi-criterial product and service comparison websites, such as
‘Which’ in the UK and ‘Tænk’ in Denmark.
Multi-Criteria Decision Analysis is the best vehicle for moving into self-produced and co-creating future and, as a completely different technique from clinical reasoning, it encapsulates the need for cultural change in medicine and medical training that goes far beyond the greater IT literacy and computer competence it also requires.